Healing Skin by altering it’s pH & microbial (Malassezia) profile
 Skin conditions such as Psoriasis, Eczema, atopic dermatitis, Dandruff, dry skin, Tinea Versicolor, Rosacea, Seborrhoeic dermatitis, Acne are in many cases thought to be caused by the fungus Malassezia.
Skin conditions such as Psoriasis, Eczema, atopic dermatitis, Dandruff, dry skin, Tinea Versicolor, Rosacea, Seborrhoeic dermatitis, Acne are in many cases thought to be caused by the fungus Malassezia.
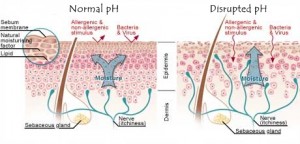
Few people know this but natural healthy skin has a pH around 4. That is quite acidic and actually a good thing. Acidic pH helps maintain skin integrity and keeps beneficial flora attached to the skin and bad flora such as fungus away. (ref.)
Malassezia grows optimally in an environment when the pH is between 4 and 8. (ref.) Therefore it is critical the skin pH be around 4 or ideally slightly lower.
The use of soaps, water, creams and makeup on the skin can alter it’s pH considerably. Washing skin with soap and water may change the skin’s pH by up too 2 points making it more alkaline and it may take over 6 hours to return back to normal baseline. Many manufacturers know this and thus “pH balance” soaps, lotions and creams to make them more acidic. And in ignorant cases more alkaline, so it’s prudent to check.
Malassezia is a lipophilic yeast meaning it eats fats and oils to make itself grow. In a lab environment olive oil is used to enhance the growth of the fungus. (ref.)
***Therefore many lotions, creams and oils used to hydrate and moisturize the skin will actually make the problem much worse despite offering temporary relief. Using most of them is like adding fuel to a fire!***
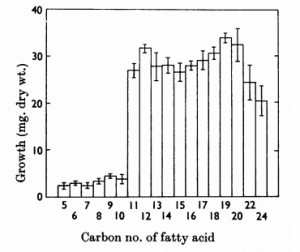
Most species of Malassezia consume fatty acids with a carbon chain length of 11 through 24. (ref.)
Therefore you want to check every single ingredient in a lotion/cream to make sure it is not within that range or else it will feed the Malassezia. For a list of oils (12-24) to avoid click here for a table.
Ointments that appear to be safe are:
- Aquaphor is 41% petrolatum, which is composed of very long carbon chains of C25 to C30
- Petroleum Jelly has carbon number mainly higher than 25 (ref.)
- MCT oil has carbon chain lengths of 8-10
Another reason olive oil is a bad for example, is that it contains Tyrosol which has been found to be a quorum-sensing molecule that accelerates the growth of the fungus Candida albicans which shares many similarities with Malassezia. (ref 1) (ref 2)
Even if the skin issue is not caused specifically by Malassezia, it may be caused by another bacteria. The following strategies will still be effective however minus the pharmaceutical antifungals. Bacteria also form biofilms, and the pH component is critical in mediating the entire skin microbiome.
Short Term Fix:
There are several strategies that can be used to kill the fungus and provide temporary relief. Keep in mind however it will grow back quickly unless the underlying environmental pH conditions skin are changed from the inside out.
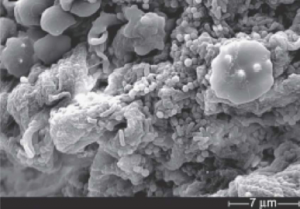
1. Breakthrough Malassezia biofilm
Malassezia as it grows forms a biofilm around itself for protection purposes. Pharmaceutical antifungals can be used but often have limited impact and will need to be used for extended periods of time due to the very slow process of moving through the biofilm.
A faster strategy perhaps is to use biofilm busting compounds. Some possible compunds are:
- Xylitol – reported by many people to be very effective, try this first
- Candex formula applied topically (1 anecdote review here)
- Chitinase because Malassezia cell wall is made up of chitn
- Fibrin enzymes such as Serratiopeptidase and nattokinase may also work
- Aloe Vera appears to also dissolve biofilms (reference needed)
- Chitosan (source)
2. Kill the fungi
- Climbazole *considered the best found in “Hegor 150”
- Clotrimazole
- Itraconazole
- Ketoconazole, Piroctone Olamine, and Lotrimin Ultra
3. Create a temporary hostile (acidic) environment so it does not grow back
- Lactoferrin inhibits adhesion (ref.)
An ideal topical lotion might contain….
- Aloe Vera gel
- MCT oil
- Xylitol
- Lactic Acid, Acetic Acid & Citric Acid
- Climbazole
- Sandalwood oil (source)
- Niacinamide (B3), plus dl-panthenol (B6) and glycerin to improve skin barrier
- have a pH of 3.5 – 4
Places to buy ingredients:
Long Term Fix:
The primary root cause of the above listed skin issues is in most cases the original use of antibiotics. Antibiotics even used once cause mass extinction on the gut biome level permanently altering the ecology which helps regulate many important functions in your body. Antiobiotics are targeted towards bacteria and in the vacuum created, often fungus take over. The goal here is to re-balance the gut biome to affect the skin. A person can affect dramatic change when using specific pre and pro biotic strategies as has been demonstrated recently with the wide use of Resistant Starch.
The most dominant variable governing skin pH appears to be lactic acid. (reference) The skin has what is called an “acid mantle” that protects against foreign invaders and helps maintain skin integrity.
So the goal here is to hopefully use the BEST pre and probiotics for increasing lactic acid in the body. This appears to be best done by supporting the growth of lactobacilli in the small intestine. Incidentally this is same strategy to use to combat Candida growth in the small intestine and in many cases it is probable that people have both internal and external fungal infections concurrently. Over growth of Malassezia on the skin is a good indicator of internal dysbiosis.
I have no idea if this strategy will increase lactic acid at the skin level, however blood pH is tightly regulated (7.35 – 7.45), so I am hoping lactic acid produced in the gut may transfer quickly to the skin if there is an adequate supply.
Many studies and anecdotes seem to suggest that pre & pro biotics can cure all manner of skin issues and I believe the lactobacilli producing lactic acid are the primary reason for this. The problem is results are often intermittent. For some people taking the probiotics alone appears to be good enough. However in more serious cases it is likely necessary to take a more aggressive approach especially if the problem is systemic. How aggressive a person may need to be I don’t know, it will be up to you to experiment.
How does skin become acidic? There appears to be several mechanisms.
- Lactic acid from microbes in the gut is taken up by blood and then released through the skin (hypothetical)
- Lactic acid byproduct from energy depletion in cells is excreted through sweat
- The conversion of phospholipids to fatty acids by enzymes in the skin (source)
The goal is to maximally produce acetic, lactic & propionic acid internally with the goal of having it secret through the skin. For a prebiotic I recommend using pectin. In prebiotic comparison studies it ferments all-around the best of many prebiotics with respect to lactic acid producing bacteria.
The prebiotic Larch Arabinogalactan has been shown to dramatically increase levels of Propionate. Propionic acid is known to be a very potent fungicide. It is used commercially to control fungi in stored grains and animal feed and has been tested specifically on Candida albicans for efficacy. (ref.)
Prebiotics recommended:
- Apple Pectin, Acacia Senegal, Larch Arabinogalactan
Probiotics recommended:
- L.Plantarum, Lactobacilli species
Acidifying Sweat:
Because tinea versicolor flares most frequently in hot climates when sweating is increased it is likely that the neutral pH of sweat is what is allowing the fungus on the skin to grow. Therefore by making the sweat more acidic it’s possible to perhaps eliminate malassezia. The following are some acids found in sweat that perhaps could be boosted with supplementation.
- Pantothenic acid aka. Vitamin B5 – ph of 4.41; is water soluble (also appears to help wound healing) (source)
- Ascorbic acid aka. Vitamin C – ph of 4.10
- Lactic acid
- serine – ph of 2.21 as a carboxyl
Skin as the last line of defense – Possible Psychological functions governing integrity of the skin boundary – a Bodynamic theory
New Theory: (April 19, 2018)
There are at least two primary body-ego functions of skin psychologically speaking and that is Energy Management and Boundaries. Skin is the boundary layer between the physical self and the environment serving the important function of differentiation. At an emotional level it is also the boundary which contains energetic-emotional energy. Developmental disruptions in childhood and/or trauma later in life can have a negative effect on these important psychological functions which then negatively affect the endocrine system that is responsible for regulating these psycho-physiological parts of ourselves.
In the Bodynamic system there are four psychological boundary layers:
- Skin Boundary
- Personal Space Boundary
- Territorial Space Boundary
- Social Space Boundary
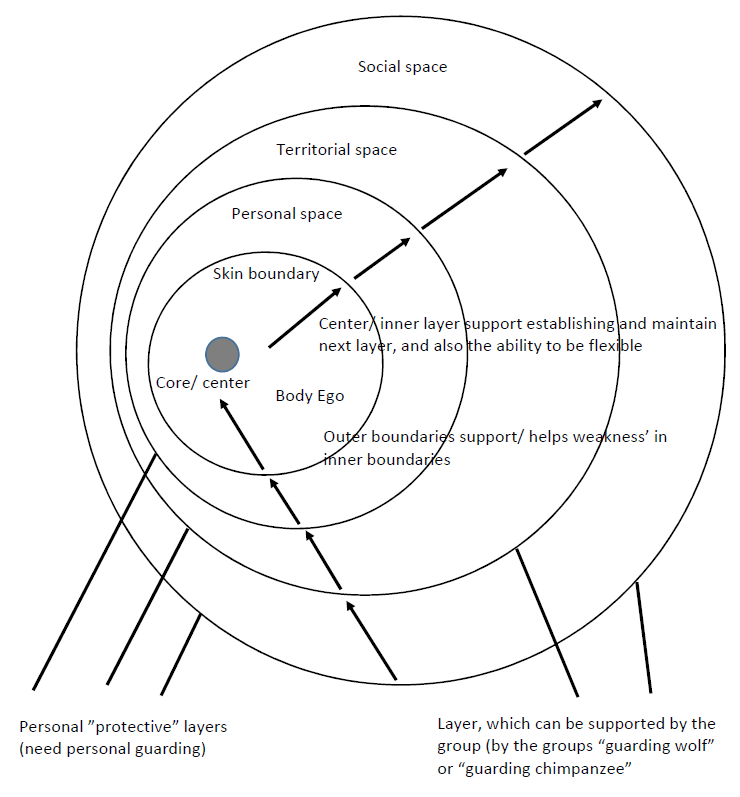
The sensi-motor development of each boundary layer occurs during different developmental time periods in relationship to the self and people in the environment. I don’t want to get into the nuances of what each boundary layer means (there is an e-course coming on the subject soon), but the important point is that gaps in boundary development and enforcement will put undue stress on other boundary layers.
For example, a parent may not have respected a child’s personal boundaries frequently overwhelming them physically or emotionally, but may have respected their territorial space. In such a case territorial space boundaries, keeping a living environment ultra organized and clean, or alternatively strewn with personal clothes or belongings is a way of using territorial boundaries to compensate for a lack of ability in more intimate personal boundary space. Kind of like a dog peeing to mark it’s territory.
If there is difficulty in differentiating personal, territorial and social boundaries the last line of separation/defense/differentiation becomes the skin boundary. The ability to sense the skin boundary and utilize it as a psychological resource is developed in utero to about 1.5 years of age. Disruptions or trauma in this age range could set up a person for having difficulty for life if the body-ego is not sufficiently developed to allow regulation of this organ.
Energy Management is another Bodynamic Ego function that could be at play here. Fascia which wrap around the muscles and are the layer between muscle and skin are psychologically responsible for containing high levels of energies and emotions. Prolonged trauma or stress can adversely affect this important layer as it becomes over-utilized in order to manage difficult emotions inside the self. This well then have a negative effect on the endocrine function in associated areas.
Bodynamic bodymaping can be used as a tool to determine how well the muscles and fascia are functioning from a psychological developmental perspective. With future correlative research (which I hope to personally engage in) it may be possible to establish causality for the psychological reasons that underlie skin issues where there is a breakdown in integrity and function. This may also help explain why skin issues show up in different parts of the body, like the hands, arms, face scalp for example. Muscles and fascia in each parts of these body areas serve a specific physiological and psychological purpose.
The tricky thing here is that it may not be the affected area where the actual problem is. It may just be the area where there are actual resources that are being over utilized and compensating for a lack or resources elsewhere. This is why getting a full bodymap done, and taking a look at the whole picture psychologically and physiologically is important.
Old Theory: (Decreasing Sebaceous Gland activity – Psychological endocrine factor – a Bodynamic theory)
It is well known that hormones (such as androgens aka. “male aggression energy”) affect SG activity. Therefore emotional stress and the physiological neural preferences could have an impact on localized skin issues. See my bodymap for further analysis. Muscles and fascia that are hypo-tonic signify areas of the body that are pyscho-emotionally inadequately brain-neural mapped in the limbic system. They are energetically under-resourced, and the lack of containment and function, likely results in undesirable leakage of said energy.
Sebum is a mixture of fats, and releasing to many be a sign of poor energetic emotional containment. Emotions as opposed to thoughts are denser energetically and are symbolized biochemically by fat, where thoughts could be biochemically symbolized by glucose. The skin ideally acts as a barrier to contain emotions. This is done psychologically by sensing into the body and feeling emotional energy bounded by the skin and contained by it. For some people this skill/neural map may need to be learned, and it’s possible this may have the effect of decreasing hormonal activity at the skin level and therefore SG activity reducing triglyceride leakage or unnecessary expulsion.
Acidity could also be symbolized by aggression energy, and a lack of containing and nurturing aggression energy could lead to an alkaline/more permeable skin barrier. Aggression is an important life force factor, one that too many people “leak out/expel” emotionally due to fearing it’s power, or bad beliefs around it. New neural maps will need to be created to harness the benefits of aggression psycho-somatically and hypo-tonic fascia and muscles need to be brought back online, in order to affect the endocrine-skin-barrier functional system.
Reference:
- The composition of Sweat, with special reference to the vitamins
- Analyzing and Mapping Sweat Metabolomics by High-Resolution NMR Spectroscopy (On all the surface parts of the human body examined in this work, the main constituents forming a sweat metabolic profile are lactate, glycerol, pyruvate, and serine.)
Additional Notes:
- “It has been shown in vitro that glycine stimulates the fast growth of M. furfur, and when this amino acid is exhausted, yeast cells employ tryptophan as a nitrogen source, increasing the production of indolic metabolites.” (source)
- “This was based on the observation that medium-chain fatty acids could delay the growth of the seven Malassezia species in vitro…” (source)
- “This study shows the efficacy of an exogenous NO-releasing cream in treating tinea versicolor.” (source)
- “The anatomical substrate of the epidermal barrier function, which is defective in atopic eczema, is the stratum corneum of the epidermis, a thin biological membrane that covers the whole body surface. It is made up of the keratinized, terminally differentiated epidermal keratinocytes of the interfollicular epidermis bound together by corneodesmosomes, filled with natural moisturizing factor and embedded in a lipidic matrix that is composed mainly of ceramides, cholesterol, fatty acids, and cholesterol esters. The natural moisturizing factor is formed by the degradation of fillagrin, comprising substances such as lactic acid, sodium pyrrolidone, carboxylic acid, urocanic acid, and urea. Decisive for the proper function of the stratum corneum is the maintenance of a pH gradient between its acidic outer and basic inner surfaces that motors many vital functions of this life-imperative biological membrane.” (source)
- “those authors pointed out, linoleic, oleic, and palmitic acids, which are potent growth stimulants of Malassezia species” (source)
- “The use of acidic topical preparations containing alpha hydroxy acids, such as lactic and glycolic acid, for kereatolysis has proved effective in clinical practice. The treatment of atopic dermatitis is aided by their pH regulating properties.” (source)
- “The effects of acetic acid (AA) and hydrochloric acid on S. aureus biofilm formation were evaluated in bullous impetigo and pemphigus foliaceus isolates and were both shown to decrease glycocalyx production. AA had a superior effect in reducing biofilm-associated S. aureus counts, indicating a specific effect of AA unrelated to low pH. In the clinical setting, AA 2.5% ointment was reported to reduce S. aureus counts in pemphigus foliaceus lesions…” (source)
- Meta analysis of lactic acid bacteria as probiotics for the primary prevention of infantile eczema (source)
- “The new antimicrobial hydrogel, made of 90 percent water, gloops together spontaneously when warmed to body temperature. It can bust through biofilms and kill a whole host of bacterial types, from small bugs like E. coli to large bugs like methicillin-resistant Staphylococcus aureus. The hydrogel is comprised of specially designed polymers, which are biodegradable and positively charged. When mixed with water and warmed up, the polymers self-assemble into chains, and the result is a thick gel.” (source)
Downloads:
- Review of OTC Treatments for Malassezia Skin Conditions by Tom Busby ver.3 Jan 11, 2014
- MCT Oil Shower Gel & Shampoo by Tom Busby Jun 9, 2014
References:
- Malassezia and Human Skin Diseases on Microbe Wiki
- Malassezia furfur on Microbe Wiki
- Biofilms in Dermatology
- Human Infections Due to Malassezia spp.
- The Rosacea Forum
- Tinea Versicolor caused by too alkaline skin – Elle Beauty
- Skin Surface pH: A Protective Acid Mantle
- Skin Barrier Function
Lactic Acid excreted in sweat…get full reference…. http://ebm.sagepub.com/content/29/8/1021.extract